Facial Veins
What Causes Facial Veins?
Both spider veins and bulging veins can appear on the face and they are often caused by different reasons than elsewhere on the body.
The most common reason for spider veins or broken capillaries to develop on the nose and cheeks is aging, but sun exposure, alcohol consumption, and even pressure from common activities can cause reddish, branching veins to appear.

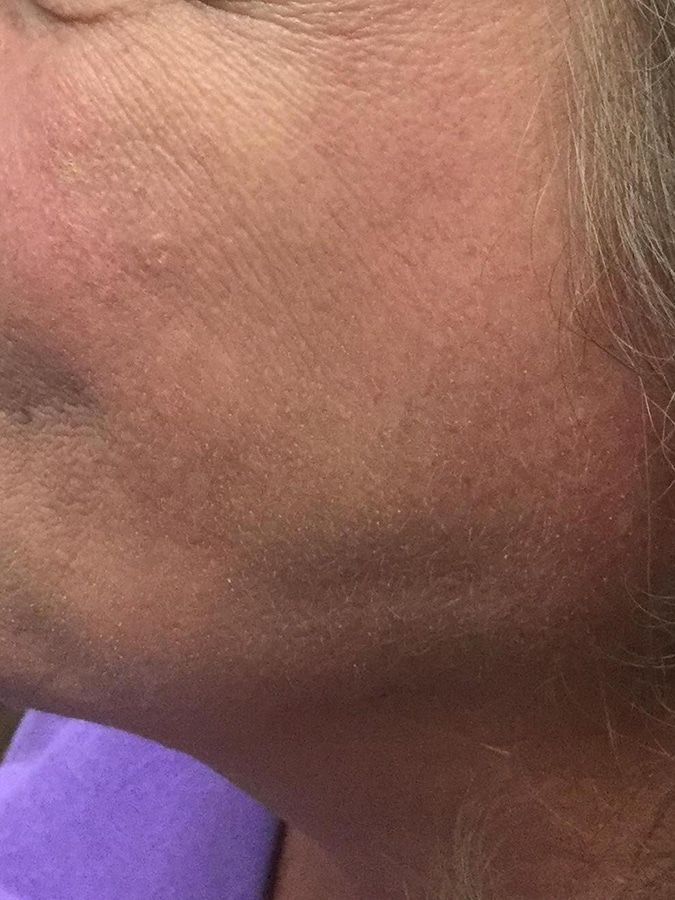
Spider Veins On The Face
Many individuals are surprised to find spider veins on their face, affecting their appearance and confidence. This article will explore the causes of spider veins on the face, highlight risk factors, and discuss effective treatments. By understanding these aspects, readers will gain valuable insights into managing and preventing facial spider veins, addressing a common concern that may impact their self-esteem. Engaging with this content can provide the knowledge necessary to take proactive steps toward healthier skin.
Overview of Spider Veins on the Face
spider veins on face, characterized by their small, dilated blood vessels visible beneath the skin, differ from other skin conditions such as dermatoymyositis. Understanding their causes is essential, especially considering factors like estrogen levels or conditions such as ulcerative colitis, which may impact the circulatory system. The following sections will delve deeper into these topics, offering insights into prevention and care, including the role of a suitable moisturizer.
Defining Spider Veins
Spider veins are small, visible blood vessels located just beneath the skin's surface, often resembling fine lines or a web-like pattern. They can occur due to various factors, including fluctuations in hormone levels, which may cause changes in blood pressure and circulation. Simple measures like wearing compression stockings and seeking therapy can aid in managing spider veins, while a professional physical examination can help determine the underlying causes and best treatment options.
Differences Between Spider Veins and Other Skin Conditions
Spider veins differ significantly from other skin conditions, such as dermatitis or eczema, mainly in their structure and underlying causes. While spider veins consist of small capillaries that become visible due to hormonal changes during menopause or conditions like type 2 diabetes, other skin issues typically involve inflammation or irritation of the skin itself. Understanding these differences can aid in appropriate care; for example, a dermatologist may recommend vitamin supplements to improve skin health while addressing spider veins with targeted treatments.
Identifying the Causes of Spider Veins on the Face
Genetic factors play a significant role in the emergence of facial spider veins, commonly known as telangiectasia. Hormonal changes, such as those affecting estrogen levels, can also impact facial veins. Environmental influences, like sun exposure, alongside lifestyle choices, including caffeine intake and poor nutrition, further contribute to spider vein development. Various medical conditions may exacerbate these issues, underscoring the importance of understanding these causes for effective prevention and care.
Genetic Factors Contributing to Facial Spider Veins
Genetic factors play a significant role in the development of spider veins on the face. As individuals age, the risk of these visible blood vessels increases due to hereditary predispositions that affect skin elasticity and circulation. Additionally, conditions causing leg cramps or prolonged sitting can lead to elevated pressure in the veins, contributing to the appearance of spider veins, even on the face. Awareness of one's family history can guide proactive measures, including the thoughtful selection of cosmetics and lifestyle adjustments to mitigate these effects.
Impact of Hormonal Changes on Facial Veins
Hormonal changes, particularly fluctuations in estrogen levels, can significantly impact facial veins, leading to the development of spider veins. For instance, during menopause, reduced estrogen may contribute to changes in circulation and increased sensitivity to environmental stressors such as sunburn or injury, which can also result in bruising. Understanding the connection between these hormonal shifts and the visibility of facial veins can guide individuals toward treatment options like ablation and lifestyle adjustments to minimize their appearance.
Environmental Influences on the Development of Spider Veins
Environmental influences play a key role in the development of spider veins on the face. Factors such as prolonged sun exposure can damage the skin and affect blood vessel circulation, contributing to visible spider veins. Additionally, stress has been identified as a factor that may aggravate conditions related to the liver, potentially increasing the appearance of these veins. Patients using topical steroids may also experience changes in skin structure, further impacting their susceptibility to spider veins. Understanding these influences can aid individuals in taking proactive measures to protect their skin and overall vascular health.
Lifestyle Choices That Lead to Spider Vein Formation
Lifestyle choices significantly influence the emergence of spider veins on the face. Prolonged exposure to corticosteroids, often prescribed for inflammation and rash treatment, can weaken skin structure, making individuals more susceptible to visible facial veins. Additionally, habits such as excessive sun exposure, unhealthy diets, and inadequate hydration can exacerbate vein appearance, highlighting the importance of maintaining a balanced lifestyle for better vascular health.
Medical Conditions Associated With Spider Veins
Medical conditions can significantly contribute to the development of spider veins on the face. For instance, individuals with skin conditions affecting blood circulation may experience heightened flushing, which in turn can lead to visible spider veins. Furthermore, weight loss can alter skin elasticity, making underlying veins more pronounced. Consulting a physician for appropriate evaluation can help identify any underlying issues and provide effective strategies for managing spider veins, particularly in relation to exposure to ultraviolet light, which can exacerbate their appearance.
Examining Risk Factors for Facial Spider Veins
Age and gender significantly influence the development of spider veins on the face, with women often experiencing these issues more prominently. Sun exposure is crucial as it can damage blood vessels, contributing to their visibility. Additionally, fluctuations in weight may affect vein prominence, making understanding these risk factors vital for selecting appropriate treatments such as laser ablation or light therapy.
Understanding Age and Gender Roles
Age and gender significantly affect the occurrence of spider veins on the face. Research indicates that women are more prone to developing visible veins, especially during hormonal shifts associated with menopause. Additionally, as individuals age, there may be deterioration in skin elasticity and circulation, leading to spider veins appearing on areas like the nose or cheeks due to increased sensitivity to heat and UV exposure. Understanding these factors can guide individuals toward effective treatments, such as laser therapy, that can target and minimize the appearance of facial spider veins associated with age-related changes or chronic diseases affecting circulation.
Advances in Laser Treatment Technologies
Recent advances in laser treatment technologies offer innovative solutions for managing facial spider veins. Modern laser options, such as pulsed dye lasers and Nd:YAG lasers, effectively target the unwanted blood vessels while preserving surrounding skin. These technologies not only improve the cosmetic appearance by significantly reducing the visibility of spider veins but also enhance patient comfort during the procedure, making them a preferred choice in contemporary dermatology practices.
Insurance Made Easier
We work with most of the major insurance carriers, including Medicare and Medicaid.
Our patients often find treatment of vein disease is typically covered by their insurance plans.
“Varicose veins are most often seen in the legs due to poor circulation and the effects of walking or standing; however, varicosities can occur in any vein throughout the body.”
Dr. Chris Malone











